Automate medical billing with Exoft
Save money with fast and error-free service
Published: 23 October, 2024 · 10 mins read
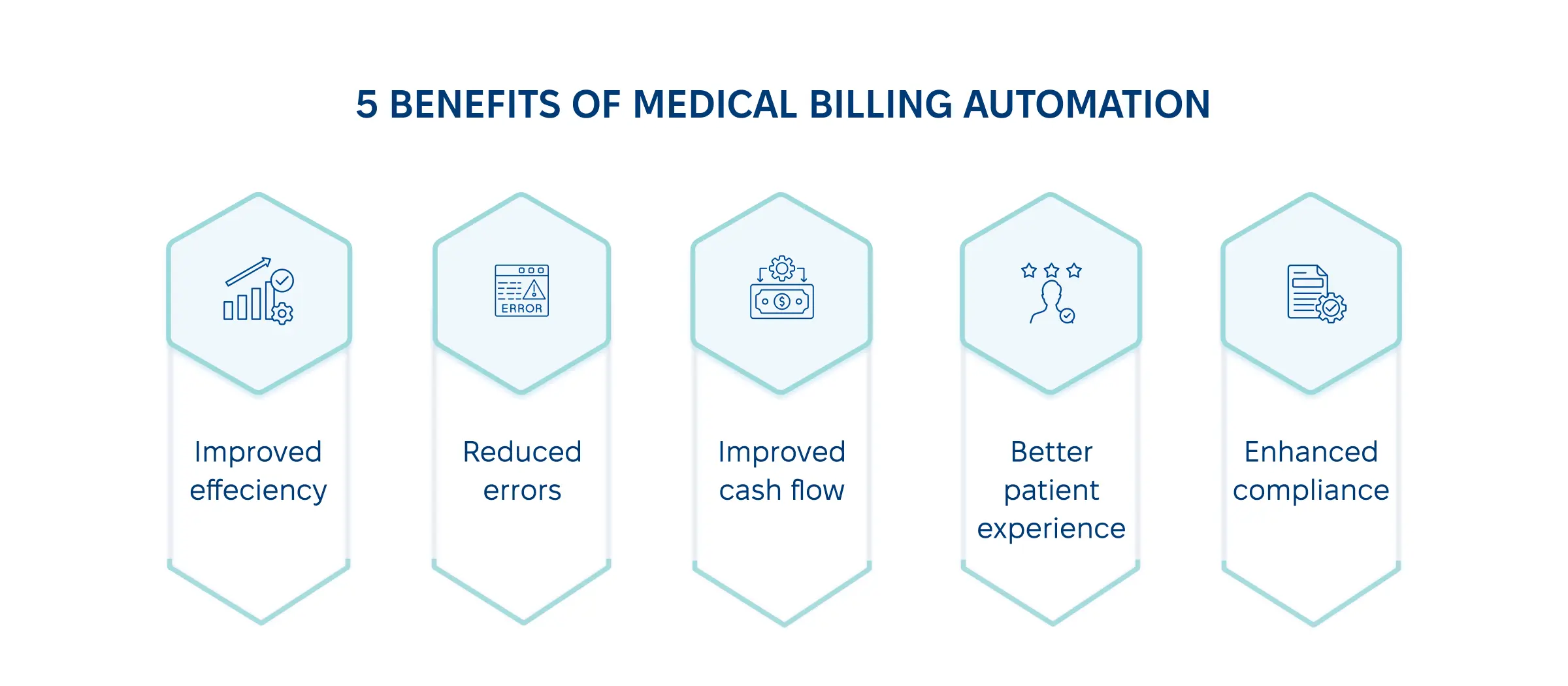
Implementing automated medical billing solutions allows you to simplify the financial aspects of your practice and concentrate on what you do best – treating patients. The benefits are immense: reduced processing times, reducing billing errors in healthcare, improved cash flow, and better patient experience. Some technologies, including RPA, AI, NLP, ML, and IDP, can aid you in healthcare revenue cycle automation. In our blog post, we discuss key stages of medical billing automation and offer 3 ready-made healthcare billing efficiency solutions suited to the task.
Being the backbone of any healthcare organization, billing ensures you get money for your services and maintain good financial health — with effective cash flow and great financial viability. In this regard, medical billing software for providers streamlines billing and is capable of creating, submitting, and managing medical bills and related payments.
In this guide, we’ll answer all the whats, whys, and hows connected with streamlining healthcare billing systems through automation:
Exoft has been working for over 10 years with healthcare providers, covering their needs in healthcare software development services with EMR/EHR solutions, hospital information systems, CRM systems, and others. From the experience of our clients, we know that it has always been a struggle to do medical billing manually. Given that around 80% of medical bills contain errors, we highly recommend making it automated — and we’re here to show you how.
Long wait times and hard-to-track random errors are the main pains for healthcare billing systems, highlighting the need for medical billing workflow optimization. Typos, wrong inputs, communication bias — all these things affect the quality of processing medical bills and block your healthcare organization from its growth potential. That’s why medical payment automation is a must in healthcare today.
With AI in medical billing processes, the automated system eliminates the human error factor, improving coding and making management faster and more accurate. This major factor leads to several less obvious benefits of automating the medical coding process.
Medical automation lets you use fewer resources for bill processing. In a healthcare institution in Southeast Asia, implementing cognitive automation in medical billing reduced processing time by 65% and automated 75% of manual effort. By streamlining workflows, the innovation lets you focus more on patient care rather than administrative routines.
When you manage hundreds of clients daily, a physician can easily miss or add an extra zero to a bill. Even if an insurance company quickly rejects wrong claims, the audit process can take weeks, if not to count administrative and legal costs and come along. That’s how a couple of typos can cost companies a million.
When you automate healthcare payments, you minimize the risk of audits and penalties associated with inaccurate billing, such as data entry errors, incorrect coding, duplicated billing, and tax calculation mistakes.
Timely and accurate billing improves revenue management, saving you time processing payments and recognizing revenue sources. As the Commonwealth Fund found out,
45% of Americans admitted they received a medical bill they thought an insurance company should cover — which is highly
unlikely to happen with medical claims coding automation.
“It’s simple math: when you make processing faster and minimize human errors to zero, you get better cash flow.”
Medical billing automation significantly improves several billing processes and improves customer service. Operations optimization makes the process hassle-free and fast for them, building your reputation as an efficient and accurate healthcare provider.
Automated medical billing software can adapt to changing healthcare regulations, making it easier for healthcare providers to stay compliant. This flexibility is essential in an ever-evolving healthcare landscape that should address the new challenges yet remain compliant with key regulations, such as HIPAA.
Save money with fast and error-free service
Automated medical billing software can use different technologies, based on your needs and benefits expected.
| Technology | Use Cases | Key Advantages |
|---|---|---|
| RPA (Robotic Process Automation) | Claims processing automation Payment posting Verification |
Reducing manual effort Minimizing errors Speeding up claim |
| AI (Artificial Intelligence) | Improving billing accuracy Automated coding |
Better decision-making Cost reduction |
| NLP (Natural Language Processing) | Working with unstructured data Chatbots |
Personalized patient experience Data retrieval accuracy |
| ML (Machine Learning) | Billing patterns analysis Coding optimization |
Learning from past data to minimize errors over time |
| IDP (Intelligent Document Processing) | Transfer of data from papers to EHR systems | Enhanced data management and reporting |
With these technologies, you can choose healthcare automation billing integration for:
In this section, we’ll demonstrate a systematic approach to automating medical billing in healthcare.
The need to go for medical billing automation may not be obvious for your healthcare organization. That’s why the first step is to prepare an effective change management plan to win top management support, communicate why it’s necessary to set automation and cover all possible concerns.
List of questions to answer:
When thinking about the ideal outcome of adopting medical billing automation services, identify the new functions you want in the system to set your budget and find a relevant software solution.
Here is the list of features and functionalities you can go for.
| Feature or functionality | What | Why |
|---|---|---|
| Claims management | Automate billing claims management in healthcare | Accelerate cash flow Reduce claims denial |
| Compliance | Keeping compliant with HIPAA and other regulatory standards | Minimize penalties Keep being up-to-date with legal standards |
| EHR systems with automated coding | Replace papers with electronic health records | Reduce human errors Improve workflow efficiency |
| Reporting and analytics | Get real-time financial reporting | Improve decision making Get accurate insights into the organization’s financial health |
| Patient communication | Automate billing-related communication | Improve patient experience with fast and accurate billing delivery |
| Security | Implement security features to protect patient data | Strengthen compliance-related efforts with patient trust |
| Revenue cycle management | Concentrate on improving the overall billing process | Detect and optimize the billing process to grow revenue |
Along with the key technologies discussed above, you should decide whether you go for off-the-shelf solutions designed to cover specific features and functionalities or build custom software that covers all your needs.
| Custom Software | Off-the-shelf Solutions |
|---|---|
| Tailored to your needs | Pre-built software with standard features |
| Personalized healthcare automation billing integration | Generally easy integration but may lack customization for your specific workflow |
| Requires more time and resources | Set price and clear expectations |
Once you choose the vendor and software type for your medical billing automation, it’s time to set the system design roadmap. Usually, your vendor’s
cooperation models
cover all the services in this step. But still, you as a client should keep the tech provider in control of getting user-friendly interfaces and meeting user experience considerations.
Here are the key workflow steps covered by automated billing:
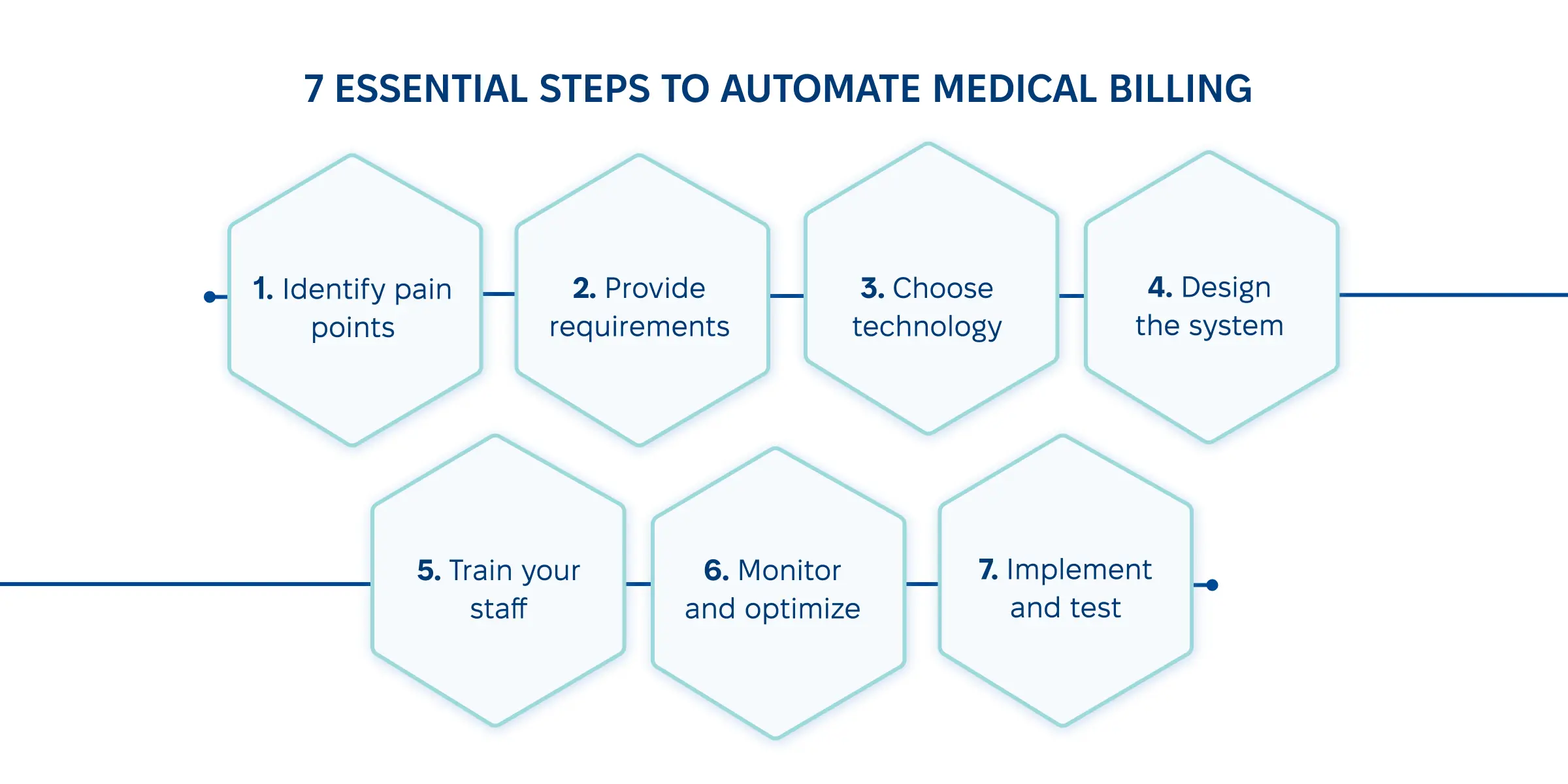
Since a professional vendor takes the responsibility of setting the implementation of medical billing automation for healthcare providers, the client needs to participate in thorough testing of all the key steps in this process, including medical code automation, compliance checks, and electronic claims submission.
The task of a vendor is to design and deliver software, but your staff will work with it afterward. That’s why it’s important to encourage your workers to participate in all the stages of automated medical billing implementation and motivate them to learn from using the new technology.
Even the
winning Telehealth strategy
cannot work without your people supporting it in your daily operations — the same applies to the best software.
As your staff keeps working with the new system, it’s your job as a manager to participate in continuous monitoring and optimization of the system. This way, the software will work for your needs and improve performance to a desired level.
On each step of implementing billing and insurance medical coding automation, concerns and obstacles can appear. In this table, we show the most common challenges from our clients’ experience and what we did together to overcome those challenges.
| Implementation Step | Challenge Example | Possible Solution |
|---|---|---|
| Pain points identification | Medical billing automation sounds great and necessary, but we don’t have money for it now | Remind the cost of doing things manually and offer a plan to spread costs over time |
| Providing requirements | We are doing fine as it is, there is nothing to change | Initiate an open discussion to make the automation benefits clear to your staff so it’s easier for them to support changes |
| Choose the right technology | Our system is too old to integrate something new | Discuss with your tech provider possible custom solutions that are within your budget and time limits |
| Design the system | Too many bugs and issues to implement automation on time | While planning automation, set extra time for unpredictable challenges. The older your system, the more extra time you’ll need |
| Implement and test | Unpredictable data security and compliance challenges | While identifying your needs, consider security and compliance as must-have elements |
| Training staff | Our staff cannot learn to operate new systems | Check the quality of training sessions and be ready to hire new people |
| Monitor and optimize | Automation doesn’t work as expected | Contact your tech provider for extra consultation |
In Exoft's experience, our healthcare clients mostly encounter challenges with maintaining data integrity, managing doctor office payments, and maintaining effective cash flow and version control.
Given our expertise in the healthcare industry, we can cover billing-related requests within
SaaS platforms and
apps, or as a part of overall
business digitalization.
Here are all the main reasons to automate billing systems:
When choosing between a custom solution and integrating a new one, consider time, cost, and your specific needs. Here are some off-the-shelf solutions you can choose from.
| Ready-made Solution | Healthcare Provider | Features |
|---|---|---|
| Kareo | Primary care | EHR integration Billing workflows Claim management Revenue cycle management Billing analytics |
| NexGen | Home care | EHR integration Billing management with support for clinical workflows Claims scrubbing and real-time tracking Voice recognition Billing analytics |
| Amazon Comprehend Medica | Hospice | NLP and ML Validation workflows Claims capture and processing Coding accuracy |
Consider that with ready-made software, it’s unlikely to get special requests covered — but with the custom software provider, you can ask for a unique solution (or a set of solutions) that can include things like
desktop or web app,
LIMS system process integration,
or even pharmacy app development!
Don’t struggle with manual errors and frequent billing delays — do things better with automation!
Whichever billing problems you currently experience — delays, human errors, or coding inconsistencies — automation solves them.
In one sentence, we’re different because we do things right (and with a 95% customer satisfaction rate!)
The exact list of automated billing system features is long, but the essential ones include automatic coding and electronic claim submission.
The exact timeframe depends on vendor capabilities and your exact needs. On average, the process takes several weeks.
Time and cost estimation depends on the type of solution chosen. For ready-made solutions, the time and cost estimation are set. A custom solution cost is negotiable and it can take up to a year.
Just relax for a while because we will contact you shortly!