Remote patient monitoring (RPM) improves treatment outcomes and cuts medical costs for patients. Hospital-wise, it reduces admissions during rush hours and yields financial gains. For these benefits to manifest, you need to develop robust RPM software, which we discuss in detail in our guide. Simply put, RPM needs a specific architectural design packed with patient- and practician-facing interfaces and responsive servers. Its most essential features include IoT-based health monitoring, patient-doctor messaging, data analytics, and data security. When developing RPM, you must consider regulations (HIPAA, FDA), legal requirements (like patient consent), and accessible design.
Around
30 million
people are expected to use remote patient monitoring (RPM) in 2024, and the market will continue to expand to
over $172 billion by 2027.
Remote patient monitoring software development can be profitable. But it’s ripe with regulatory hurdles, legacy integration issues, and adoption friction. In this post, we’ll address the core questions on how to develop remote patient monitoring software and share Exoft insights, such as:
- Aside from ensuring data security and logging patient data, developing RPM software should include communication tools and accessibility features.
- Device calibration and maintenance documentation is as vital for RPM as patients’ consent.
- Patient buy-in is critical to fast RPM adoption and long-term success, and education is vital for securing enthusiastic adopters.
For more helpful insights, check out Exoft's take on
2024 MedTech trends,
healthcare of the future,
and our experience with
SaMD.
How an RPM System May Help Optimize Expenses
A 3-day stay in the hospital can cost
up to $30,000
for people without medical coverage. So, patients would benefit greatly from remote patient monitoring software development. At the same time, RPM can also help healthcare facilities make business processes more efficient and optimize expenses. Considering the ongoing shift towards preventive care, arming doctors with RPM functionality can reduce the number of hospital admissions, freeing up resources and medical personnel.
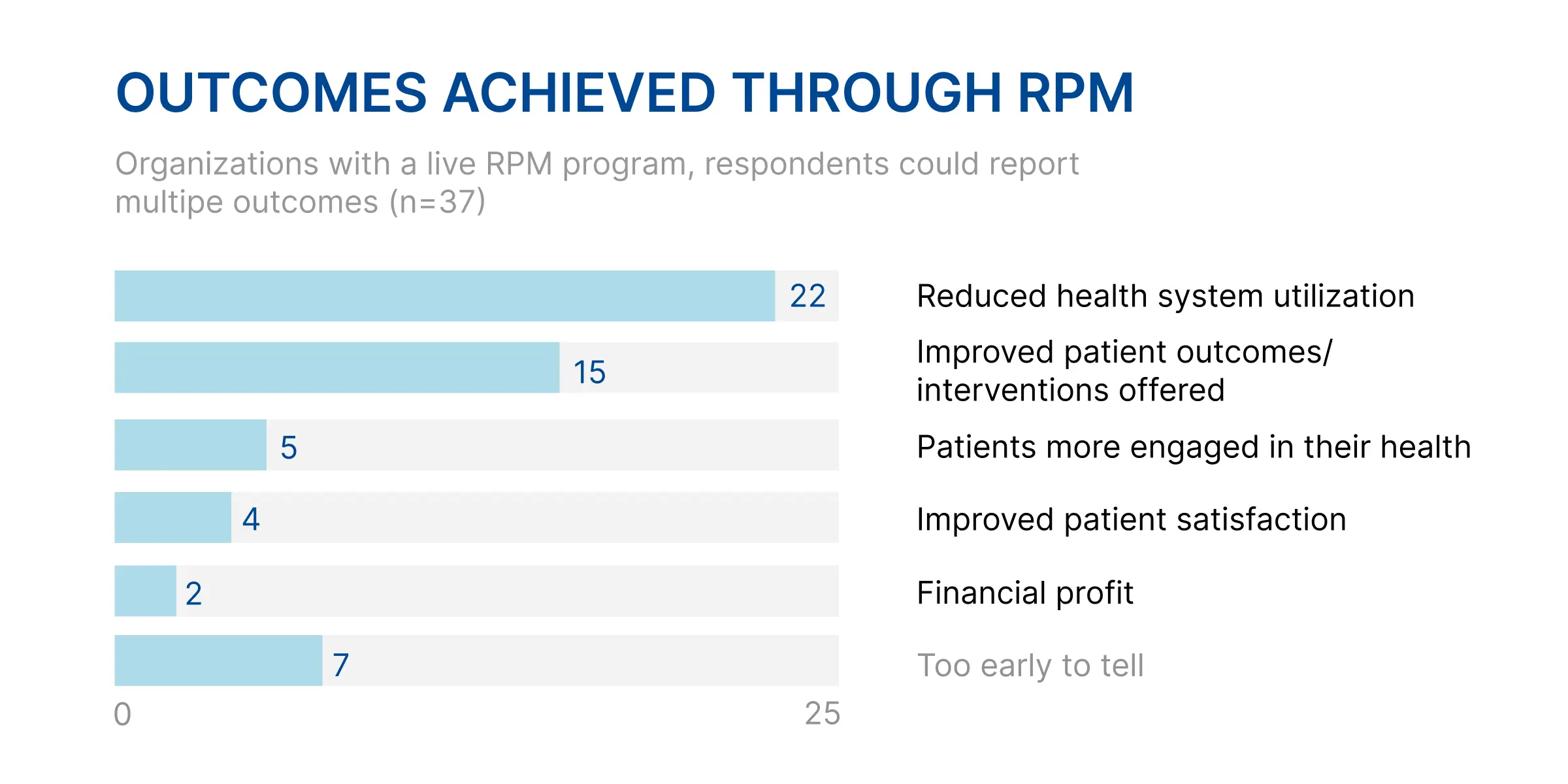
According to the Remote Patient Monitoring 2022 report,
- 22 out of 37 organizations with live RPM programs saw decreased health system utilization. This included hospital admissions and ER visits. In turn, this helped with bed availability during high-traffic periods. It can be especially helpful for rural healthcare, enabling physicians to monitor patients without long drives to the nearest hospital.
- 15 out of 37 organizations claimed improved patient outcomes. Earlier interventions resulted in better outcomes. Even if only 4 out of 37 reported improved patient satisfaction.
- 2 out of 37 organizations reported financial profit among the benefits of the RPM system. Instead, most facilities prioritize long-term care cost reductions.
Increased productivity is among other RPM benefits. One nurse can monitor over a hundred patients remotely, thus reducing the need for medical personnel. Doctors, on the other hand, can reduce the number of costly tests. Using RPM data helps diagnose and assign treatment faster.
RPM System Architecture Overview
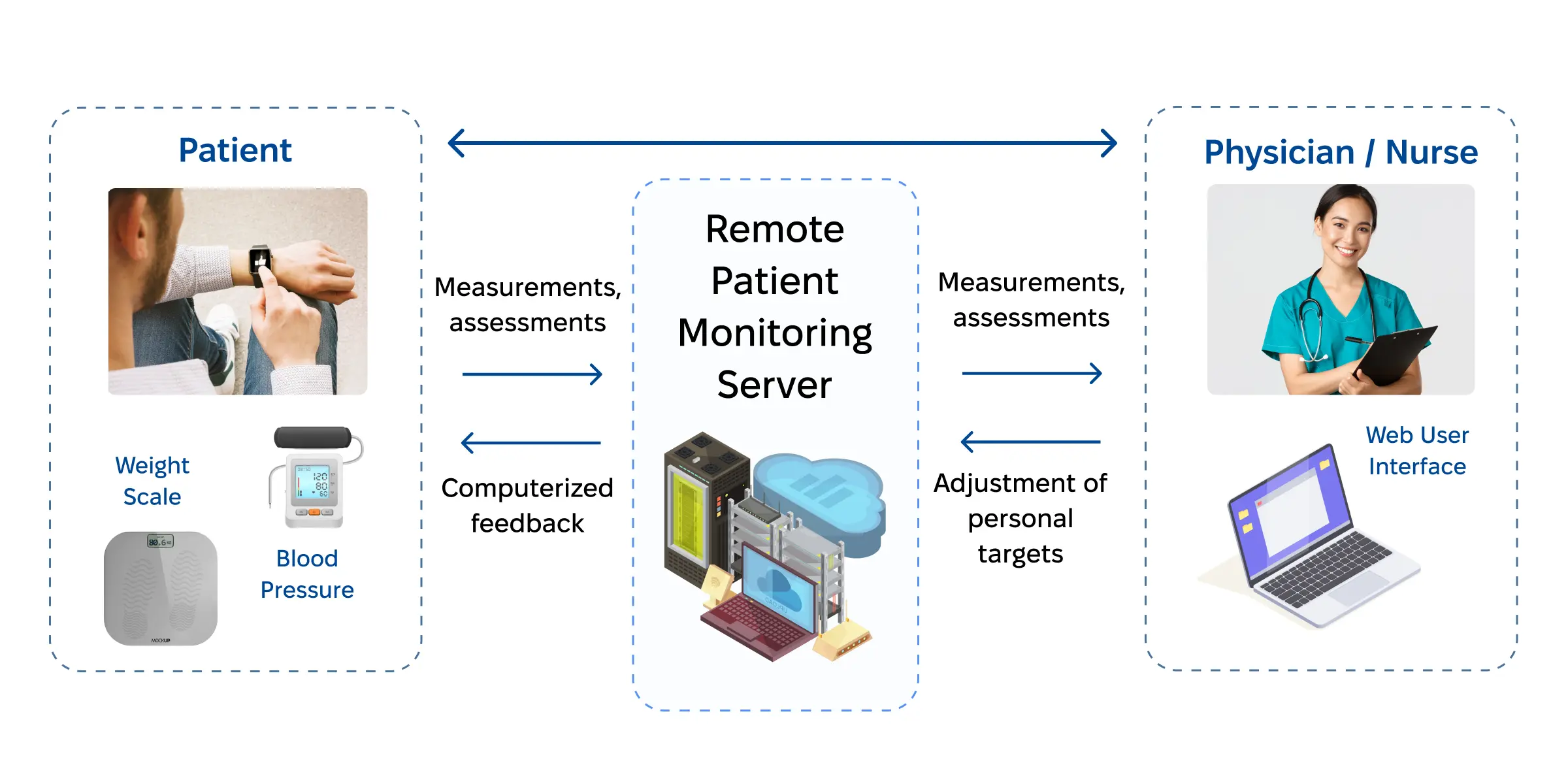
Among other things, an RPM system is designed to collect patient data and deliver it to healthcare professionals. They, in turn, diagnose issues and provide treatments or recommendations. To achieve these goals, a basic RPM architecture comprises three main components:
- The patient-facing component
can include anything from wearable monitoring devices and smartphones to a patient mobile app. Its main goal is to collect patient healthcare data and deliver feedback.
- The physician-facing component
is usually a mobile or web app that lets doctors and nurses assess patient measurements. Physicians can also adjust treatment plans and deliver updated recommendations.
- The RPM server
collects and stores data from the patient-facing and physician-facing components of the patient monitoring system. Medical professionals can use it for computing and to access historical data. Administrators can assess healthcare outcomes and patient satisfaction rates to improve managerial decision-making.
Core Features of Remote Patient Monitoring Systems
The list of features for remote patient monitoring software development will depend on the type of solution you want to build.
IoT-based Patient Monitoring
Wearable healthcare monitoring devices are at the core of the patient-facing RPM component. Advanced IoT-based patient monitoring software solutions should:
- Integrate multiple wearable monitoring devices
- Enable patients to log their symptoms manually
- Enable patients to log medicine intake
- Log patients’ physical activity, sleep, and health data
- Set up device failure and maintenance alerts
Patient-Doctor Communication
A communication toolset is not a requisite among the features of remote patient monitoring systems. However, it is relatively easy to implement and tends to garner positive patient feedback. These are the two most common tools you can use:
- Chat is a suitable solution for non-urgent patient requests.
It’s a convenient way for patients to contact physicians between appointments.
- Video or audio calls can partially replace in-person appointments.
Unless a hands-on examination or physical therapy is required, physicians can assess changes and adjust care plans through virtual visits.
Running patient-doctor communication through the RPM system can also benefit healthcare professionals, as they can log additional hours and use records as evidence in case of patient complaints.
Data Analytics and Reporting
An RPM system development for hospitals would be incomplete without a physician-facing component. Here are a few features it should include:
- Setting up reference parameters for individual patients for comparison with real-time vitals.
- Identifying trends in the patients’ symptoms and treatment.
- Analyzing vitals over a specified period and comparing them with current data.
- Setting alerts for alarming vital numbers for immediate contact and dispatching urgent care.
- Generating patient status and treatment plan reports for healthcare institution internal reviews.
Data Security
Aside from regulatory compliance with HIPAA, RPM solutions should also account for:
- Role-based access for users of different tiers.
To prevent data breaches and leaks, administrators, physicians, and patients should only be able to access data pertaining to their roles.
- Data encryption.
It’s critical for patients’ personally identifiable data, as well as appointment times and recordings.
- Multi-factor user authentication.
Along with strong password requirements, it’s an industry standard for accessing any system dealing with sensitive information.
Accessibility Features
Accessibility features are often overlooked during remote patient monitoring development. These can include text-to-speech and speech-to-text functionality for people with impaired vision. Voice search and controls can be equally helpful for them and patients with motor dysfunctions.
Documentation Requirements for Remote Patient Monitoring
Regulatory compliance and proper documentation are critical if you wish to build a remote patient monitoring system. Let’s go over the legal challenges you’ll face in the US and core documentation requirements a RPM solution should meet.
RPM Regulatory Compliance
Ensuring protected health information (PHI) security is among the key challenges for any MedTech solution, including telehealth systems and RPM technology. Still, it’s not the only regulatory hurdle you’ll need to overcome.
- Health Insurance Portability and Accountability Act
(HIPAA)
is the core federal regulation RPM systems must follow. It’s designed to protect patients’ privacy and ensure their data is secure. Your organization must develop and adhere to policies and protocols for data encryption, access rights, and breach response.
- The Food and Drug Administration (FDA)
issues approvals for the use of noninvasive health monitoring devices. To comply with federal regulations, it’s critical to add FDA-approved IoT components to your RPM systems. The complete
list of approved devices,
along with the list of
recent recalls
and banned devices, can be found on the FDA website.
Non-compliance is expensive. For example, every case of criminal HIPAA violation can cost your organization between $50,000 and $250,000. According to the
Department of Health and Human Services, OCR has ruled penalties in 145 cases, resulting in overall fines of over $142 million.
To avoid regulatory losses, contact Exoft to learn more about our experience handling regulatory compliance in
healthcare software development.
Primary RPM Documentation Types
Patient Consent Paperwork
Before implementing an automated RPM platform, you must obtain patients’ explicit consent. They must consent to you collecting, transmitting, storing, and processing their PHI. You must clarify what types of information you plan to collect and how it will be used. You may also need to share the security measures ensuring PHI security. To cover your bases, document patients’ questions and concerns. Provide regular updates in case of any changes in your information-handling policies. It should keep your consent process transparent while protecting you from legal challenges.
Device Calibration and Maintenance
Physicians require accurate healthcare data to diagnose and treat patients. That’s why device integrity and proper operation are critical. You need to document every calibration, maintenance, and repair RPM devices undergo. Note the date, time, types of tasks performed, and people responsible for the jobs. Careful documentation can help you uncover malfunctions and other issues. It ensures correct operation of the RPM system and improves patient satisfaction.
Patients’ Health Data
Patient's vitals are an integral part of patient monitoring software solutions. But for maximum efficiency and safety, RPMs should amend the raw vitals collected via wearable devices with:
- Symptoms and complaints the patient reports
- Healthcare data analysis and interpretation by medical professionals
- Followup communication logs between the patient and physician
Such datasets will provide healthcare professionals with enough information to make informed decisions about developing or adjusting treatment plans. Organizations can also use this data for training, improving personnel management, and other internal business processes.
Design Considerations for RPM
There’s no universal template for best RPM software development for hospitals. Still, using current industry best practices is a good place to start:
- Develop an intuitive user interface.
Many patients with chronic conditions are within the 60+ age bracket. They can have trouble navigating a web or mobile app. You need to make it comfortable and easy to navigate for users of all ages. Have older people test your UI and follow their suggestions before implementing the design.
- Remember about accessibility.
Voice commands, text-to-speech, and other accessibility features will help users with trouble typing or vision or motion dysfunctions.
- Keep battery requirements manageable.
Limit the background processes and focus on low-energy solutions, such as the latest version of Bluetooth or the dark mode.
- Implement offline capabilities.
Patient data shouldn’t be lost when they don’t have an internet connection. Ensure your solution has cashing capabilities to store real-time data that will be transferred to the cloud or server once the connection is reestablished.
- Enable precise geolocation.
Patients won’t appreciate physicians tracking their movements. However, sharing their exact location in case of a medical emergency can be key to saving their lives. Create an RPM software platform that allows users to request urgent help and sound the alarm with a tap.
- Use security-first design.
Staying HIPAA compliant is much easier when every UX design decision is guided by security precautions. It can be as easy as integrating password validation to ensure it’s long and complex enough to prevent brute force breaches.
- Manage notifications.
Flexible notification management is critical to lower patient frustration. Still, patients should receive regular updates on their vitals. Physicians should be immediately notified of any abnormal readings.
Finally, building a remote patient monitoring system that seamlessly synchronizes data across multiple wearable devices is a must. Patients, physicians, and admins should be able to access the RPM system from any desktop or mobile device.
Risk Management in RPM Development and Implementation
According to a
2023 systematic review,
building software for remote patient monitoring and its implementation evoke the following challenges and risks for healthcare organizations and professionals:
- Increased workload.
Healthcare professionals believe the volume of patient data can become unmanageable, especially if it’s not integrated into electronic medical records. However,
future healthcare
automation through machine learning and artificial intelligence algorithms can help mitigate adoption friction.
- Questionable data accuracy.
Physicians tend to trust wearable personal medical device data less than that of specialized medical hardware. Besides, patients may not be using devices correctly to produce valid results. Patient training techniques and widespread adoption of wearable MedTech can reduce this risk.
- Technological illiteracy.
Handling wearable devices and smartphones can be challenging for older patients who need remote monitoring the most. However, healthcare organizations can mitigate this risk by developing RPM software with intuitive controls and by normalizing the devices used.
- Financial concerns for low-income patients.
Accessing RPM-supported devices can be beyond their budget, limiting their access to quality healthcare. At the same time, as RPM can reduce the number of hospital admissions and resultant costs, purchasing RPM devices can be seen as a long-term investment.
- Privacy breach concerns.
Physicians, hospital administrators, and patients are concerned about personal data stored by third-party software. HIPAA compliance is critical for dispelling these reservations as well as avoiding legal repercussions of user complaints.
Overall, medical professionals and patients consider remote patient monitoring technology a relevant tool despite their reservations. Understanding and addressing these concerns while building software for remote patient monitoring is necessary to reduce adoption friction and realize the solution’s full potential for reducing expenses and improving healthcare outcomes.
RPM Deployment and Post-Launch Considerations
After the final round of testing is finished, the remote monitoring system development is done. Only launch and deployment remain, but this part of the process is equally critical for RPM's long-term success. At this stage, you should focus on integration and training.
Personnel Training
Instruction manuals, video tutorials, and hands-on workshops should be enough to prepare healthcare professionals to use all of RPM’s features. However, ongoing support for addressing issues arising from real-world use cases is necessary.
Moreover, medical staff will also need basic cybersecurity training to handle sensitive patient data and prevent RPM data breaches. As human error is the most common cause of data breaches, healthcare professionals need reminders on how to create complex passwords, why multi-factor authentication is important, and what to do in case of a security breach.
Patient Education
Patient buy-in is the deciding factor in the successful launch of an RPM platform. It isn’t enough to build a remote patient monitoring system; you need to convince the patients to sign up. Without their explicit consent, an RPM will go to waste. Therefore, medical professionals should explain what an RPM is, how it works, and how it can help patients improve healthcare outcomes. Reducing hospital admissions and the cost of healthcare are often the deciding factors for patients, though some value active participation in the treatment process or increased collaboration with healthcare providers.
After the patient buys into the RPM program, you’ll need to educate them on the proper use and maintenance of wearable devices. Nurses and orderlies can deliver preliminary hands-on training, while further education can continue at home through different channels.
Ongoing Technical Support and Maintenance
Early days of implementation often highlight the shortcomings of remote patient monitoring app development. Ongoing maintenance and continuous upgrades post-launch can help resolve these issues and keep physicians and patients happy. Moreover, ongoing support should include security upgrades to remove vulnerabilities and ensure PHI safety under the terms of HIPAA. That’s why choosing a reliable remote patient monitoring software development company should be a part of your long-term
telehealth strategy.
The Bottom Line
Medical professionals recognize RPM as a valuable tool for improving healthcare outcomes. It can reduce hospital admissions and readmissions, lower medical costs, and increase medical personnel efficiency. Still, remote monitoring system development raises many concerns and requires an in-depth understanding of the regulatory requirements, diverse use cases, and legacy systems integration.
Exoft.net is a
product development service
with proven expertise in developing healthcare solutions, including telemedicine and health metric systems. To learn more about the Exoft HealthTech experience, check out our
case study
library and contact us for a consultation on building a remote patient monitoring system.
Frequently asked questions
What are the key regulatory challenges of RPM development, and how can you help navigate them?
Failure to comply with HIPAA and FDA requirements can result in fines and reputational hits. Our familiarity with federal regulations ensures a security-first mindset throughout remote patient monitoring software development. Industry-standard encryption, MFA, and personnel training ensure PHI security.
What is the typical timeline and cost of developing a custom RPM solution?
The pricing and timeline for an RPM solution depend on your specific requirements. Initial investments for a startup can range from $5,000 to $20,000, with ongoing monthly maintenance and upgrade fees. The discovery stage can take up to a month, while the remote patient monitoring app development process will take at least three to four months. Testing, release, and launch can also take a few weeks. Overall, you can have a live RPM solution in six months, though complex projects will take longer.
How do you ensure data security and patient privacy?
Exoft employs RPM software development best practices to ensure data security and patient privacy. They include end-to-end data encryption, multi-factor authentication, and multi-tier access hierarchy.
How can remote patient monitoring affect our income and spending?
RPM is proven to reduce healthcare costs through improved outcomes and fewer hospital admissions. Some organizations see an increase in profit, but most invest in RPM software development to achieve long-term savings.