The healthcare industry uses technology to solve its most pressing problems, like patient dissatisfaction, negative margins, and big data management. However, to move from reactive to preventive medicine, innovations must transition from experimental pilot projects to routine practice. Our blog post discusses solutions with the greatest potential for future patient care, from integrated digital healthcare to data interoperability and predictive analytics.
Introduction
Digestible sensors? VR treatment? mRNA vaccines? Artificial organs? Blood tests for depression? Gene-editing therapies? Medical tricorders?
While some of these technologies exist already, more effort is needed to evolve them from ‘cool tech’ to beneficial, routinely available diagnostics and therapies ready to transform healthcare.
In the medical innovations world, there is no shortage of promising technologies, but there is also a lot of hype. There is no question that technology can change the way medical services are delivered. It’s “how” health-related issues can be addressed with technology in the best way. However, it is still fundamental that no matter what you make or sell, it’s still about the people.
With recent global pandemics and current economic turbulence, digital health has become a reality check for everyone involved, healthcare providers, patients, pharma researchers and technology vendors.
Technology is forging new standards for what the integration of customer experiences and healthcare digital innovation can achieve. With the nexus of instruments that we have today, more and better data than ever before, next-gen platforms, lightning-speed connectivity, knowledgeable and active consumerism, access to services at the fingertip, there is still something missing. While the medical sector is more open to adopting digital healthcare to improve outcomes, bureaucracy, money, or reluctance to change still tend to get in the way. As a result, the domain is facing drastic issues.
- Patients expect more from their healthcare providers.
73% of adults feel that the healthcare system fails to meet their needs in some way (The Harris Poll on behalf of AAPA – the American Academy of Physician Associates). - Healthcare providers are challenged with revenue cycle efficiency.
43% of Community Health Centers operate on negative margins (Health Affairs study). - Health systems are approaching data management paralysis.
30% of the world’s data volume is generated by the healthcare industry (RBC Capital Markets).
Both technological future enthusiasts and health services pragmatists agree that while there are some changes now, the industry is rushed towards even more developments.
Healthcare is Pushed to Invest in Technology Innovations
Traditionally, the healthcare industry is not designed nor prepared for such an influx of new technologies as we see arriving today: from healthcare workers shortage, medical care access and affordability gaps, ethical and legal inefficiencies to care approach, financial strains on the public health system, low insurer reimbursement rates, non-compliance with healthcare privacy and security regulations.
On the other side, there is a digitally driven patient, immense automation opportunities, pharma research breakthroughs, data-based ecosystem interoperability, novel therapies, machine intelligence, and, of course, a crying demand for affordable quick efficient care with a revenue-generating new business model approach.
The global healthtech experts highlight many drivers for the future development of health care. Here are some key ones:
Technology Innovations Bring New Possibilities
From a business standpoint, the medical industry has to connect the dots. Isolated digital innovations in healthcare drive only limited progress. Taking a holistic perspective on the healthcare industry as an ecosystem though, does. To survive in this healthcare sector’s dynamics, providers must centralize patient data, track patients’ therapeutic journeys from start to finish, measure outcomes that matter to patients and make use of digital transformation and emerging technologies to improve the medicare experience and, consequently, physician’s practice ROI.
So what will a new business model of the healthcare of the future look like?
Integrated Digital Healthcare
Digital technology is inducing a new norm for the healthcare industry removing fragmentation and focusing on the care continuum. Applying digital innovations in healthcare makes it an integrated journey for patients, a coordinated facet for providers as well as a measurable efficiency of the medical system on the whole.
Integrated digital healthcare is the alignment of digital tools, platforms, software solutions and data sources in healthcare systems, like Electronic Health Records (EHR) , Telehealth & Telemedicine, Health Information Exchange (HIE), Mobile Health (mHealth), Data Analytics, Artificial Intelligence (AI) technology application, and Patient Engagement and Empowerment tools.
It has the potential to completely revamp the sector in terms of providing better access to medical services, improved treatment outcomes, streamlined patient satisfaction as well as reduced expenditures throughout the entire healthcare process.
«Coordinated treatment of patients with diabetes, hypertension, asthma, or arthritis leads to $656 million in savings, according to the Sustaining Healthcare Across Integrated Primary Care Efforts (SHAPE)»
Interoperability and Data Sharing
With an explosion of human digitization through new devices, monitoring technologies, and apps that are tracking, generating, and analyzing massive amount of information, on top of traditional medical records, data – is turning into an asset for medical sector – transforming it from care to health, from treatment to prevention, and from investment to profit at the end of the day.
Sharing, integration, and utilization of the so-called “data-ome”(personal data accumulated from every source point) across various platforms and organizations will allow for holistic analysis of the information to gain insights into individual health, population health, or disease mechanisms.
«82% of healthcare providers consider data interoperability essential for improving patient care, and 63% believe that it is key for reducing healthcare costs (The Future Health Index.)»
Though still in infancy, governments and industry organizations are starting to dismantle data barriers to achieve data interoperability. The most vivid examples are the adoption of standards and data sharing initiatives such as Health Level Seven International (HL7) and Fast Healthcare Interoperability Resources (FHIR), the 21st Century Cures Act by the US National Coordinator for Health Information Technology(ONC), as well as UK’s Biobank or My Health Record in Australia define common data formats and structures, allowing systems and individuals to exchange information securely, consistently and efficiently.
Healthcare businesses are also adopting APIs to connect disparate systems, integrate data from multiple sources, and enable seamless data sharing between different healthcare applications. Although, regrettably, such ‘point to point’ integrations often ignore data exchange protocols such as HL7 and FHIR, and it could be argued that they are counter-productive to the larger goals in integrated healthcare.
Cybersecurity & Data Privacy in Healthcare
When it comes to digital in healthcare, personal information is being pumped in exponentially. Though far from being a cure for all illnesses, cyber defense and the need to deal with data as a property which has to be stored, secured and protected is today pushing the medical sector to embrace technology.
With global privacy regulations such as the GDPR and HIPAA growing in importance, health systems are striving to maintain compliance while constantly evolving their cybersecurity strategies. Also, healthcare organizations are increasingly investing in staff training and awareness programs to educate employees about phishing attacks and other potential data breaches.
«Healthcare companies spend $39 billion annually on regulatory compliance.»
Recent developments in healthcare cybersecurity include the adoption of multi-factor authentication, advanced threat detection, and the deployment of AI-driven security measures. From secure patient communication methods (like encrypted messaging platforms or consent management systems) that enable controlled access to patients’ data to futuristic Blockchain technology for data storage and transactions – companies and governments are seeking ways to address the ever-evolving threat landscape.
On top of that, the cloud age is ripe with opportunities for healthcare to secure the environment and keep sensitive patient data protected from external threats. Additionally, the implementation of mobile and IoT device management strategies are already working towards enhanced security for accessing confidential patient data.
Artificial Intelligence and Machine Learning in Healthcare
Driven by the need to improve healthcare and reduce costs, AI and machine learning are very much here and today. Though the industry as a whole is evaluating how best to adopt these technologies, it’s already moving from enigmatic big data to actual knowledge and ultimate intelligence: from early detection and diagnostics to clinical decision support, medical imaging, drug discovery, personalized medicine and remote monitoring, to outcome prediction and robotic surgery.
Not only bigtechs like IBM, SAP, Oracle, and Microsoft jumped into their own AI healthcare projects, hundreds of helthtech trailblazers have started creating tools to aid health systems with machine intelligence.
Source: Statista
Despite some ambiguity in regulation for e-medical software as well as the lack of skilled AI workforce, machine learning, deep learning, and image recognition are some of the AI applications used in healthcare on a daily basis. As much as AI-based technologies have already done for administrative tasks automation and efficiency and effectiveness of healthcare operations, legacy healthcare data management systems and medical imaging processors modernization, the medical sector is focused on advancing disease identification and diagnosis with AI.
«The most common types of AI software in use in healthcare worldwide in 2021 was healthcare data integration and natural language processing. (Statista)»
AI has already demonstrated its effectiveness in monitoring and predicting global health epidemics, as evidenced by a computer algorithm identifying an Ebola outbreak nine days prior to its official report by the World Health Organization.
It’s safe to say that implementation of AI in more areas of medical care will be among the top trends in digital healthcare in the coming years. Machines are now learning how to read imaging diagnostic tests to identify abnormalities and serve as virtual nurses and surgical robots. From cancer to mental health, AI algorithms are changing the game within disease diagnosis.
By extracting more meaning from data across clinical trials, AI has the potential to facilitate development of DNA-based customized drugs. The use of generative AI accelerates the drug discovery process, identifies repurposing of current medications, improves the efficacy of drug synthesis, and predicts side effects, thereby reducing costs and time-to-market for new medications.
AI-powered simulations, augmented reality (AR), and virtual reality (VR) technologies are now being looked at to enhance medical training for healthcare professionals by offering realistic scenarios that mimic real-life situations.
Remote Patient Monitoring in a Personalized Way
In an economy where everyone is under inflation-driven financial pressure, patients-consumers are seeking more value for their money which means getting the best experience possible. While ensuring speed, accuracy, consistency, and security, AI has a potential to move medical treatment away from general, one-size-fits-all options to more personalized solutions.
«When a healthcare provider does a good job of personalizing customer interactions, 49% of patients feel like they care about earning their business and 47% are more likely to choose them. (Invoca)»
Machines have inherent advantages over humans in probabilistic, computational or data-heavy tasks essential for diagnosis and clinical triage, behavioral monitoring and keeping pace with the latest treatments. It means that by combining meaningful human interactions and data-based methods, healthcare can create a more patient-centered approach to care that fosters lasting relationships between the two. So, machine-powered intelligence allows the providers to exchange and act on individual patient information for improved care coordination, enhance clinical decision-making, support research and population health, and most importantly engage patients in their own health decisions.
For instance, conversational AI in healthcare (backed by deep learning and natural language processing – NPL) is turning into an accessibility tool enabling quality personalized experiences for many patients and providers. Be it self-service or appointment management, intelligent symptom check or post-treatment care, public health information distribution or health tracking – speed, accuracy and productivity will likely move on to supercharging patient experience and help move on from click to call to conversion.
Likewise, generative AI is making huge strides towards supporting personalized treatment regimens by instantly analyzing patient data based on medical history, genomics, and proteomics. This approach to customized healthcare is likely to prevent adverse reactions and improve outcomes much quicker and at lower cost.
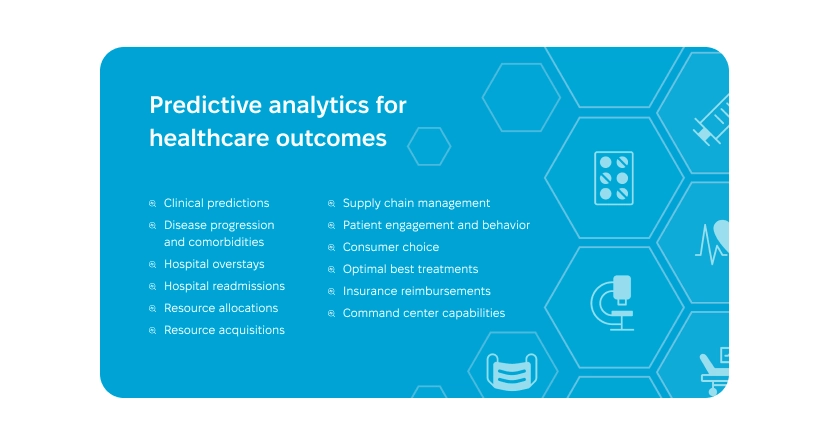
Predictive Analytics in Healthcare
One of the supernova uses of AI in healthcare is in the world of predictive analytics. It has already entered clinical research and pharma labs and the new use cases of predictive analytics in digital health services are on the way to improving patient care outcomes. Powered by big data, it’s taking on a significant role across resource management, patient engagement, insurance reimbursement, and patient choice of providers. Also, AI-powered predictive analytics is looked at as a marvel for medical professionals to develop a better scientific understanding of the incubation and spread of infectious diseases in the future.
The personalization aspect of wellness is another important area where predictive analytics is potentially making a difference. Predictive analytics can process individuals’ data to create personalized health plans like exercise routines, dietary guidelines, medication plans, etc., that take into account their specific needs and preferences.
However, the most realistic application scenario for predictive analytics in the future of healthcare with the limited dollars to invest in the continued innovation without visible returns, is the health system’s overhaul of the cost efficiency of both the clinical care together with supply chain and logistics. So that it’s possible to carry out preventive care in the first place, and provide effective and affordable healthcare to those who need it precisely when they need it.
That’s why from where we are now, leveraging data analytics combined with practical experience and personalized approach to well-being is the most feasible development of preventive care. With the data available from electronic health records, wearable devices, genetic testing, healthcare providers can effectively predict when an individual is edging closer to conditions like diabetes or obesity, among others, by leveraging data analysis, without necessarily launching costly and elaborate AI projects. The beauty of predictive analytics extends beyond diagnosis – by tailoring wellness plans according to individual requirements, the patients can receive the most effective targeted preventive measures that will improve health equity outcomes and essentially reduce healthcare administrative costs.
Telehealth and Remote Patient Monitoring
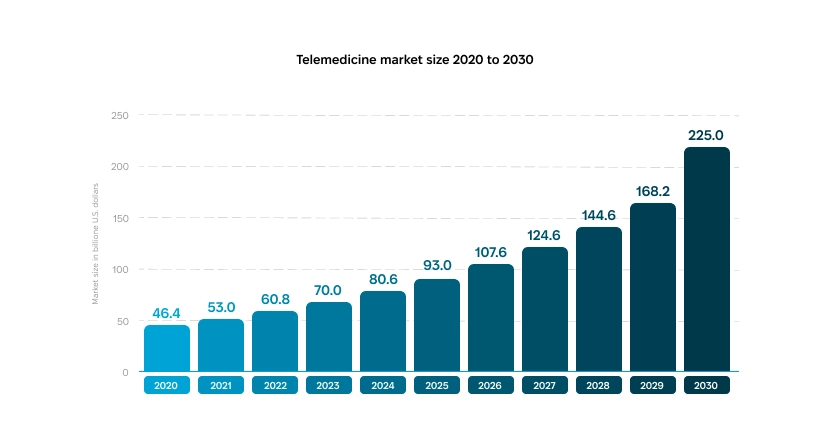
Telehealth services and telemedicine have existed for years, but it was the COVID-19 pandemic that has turned virtual care into a mainstream method of receiving the right services at the right place and at the right time. The connected world of digital transformation makes it easier to reach the doctor at our fingertips making it one of the most widely accepted trends in digital healthcare without any signs of slowing down.
It has become evident that telehealth can enhance efficiency in general and urgent conditions care specifically, optimize time and costs, expand care accessibility, and alleviate the burden on healthcare facilities by minimizing patient demand.
«Younger American doctors consider telehealth as a more valuable healthcare technology compared to AI. In their opinion, telehealth technologies (with a combined percentage of 55%) would have greatly enhanced their working experience during the COVID-19 pandemic, surpassing AI technologies (41%). (The Future Health Index)»
Moreover, through proactive healthcare measures, telemedicine can help prevent unnecessary emergency department readmissions by engaging patients more frequently and at a reduced expense. So, it’s obvious that we are going to see tremendous investment in telemedicine and virtual patient care in the near future.
The global telemedicine market is expected to reach USD 225 billion by 2030, compared to USD 60.8 billion in 2022.
Looking into the future, the industry experts are expecting telemedicine with add-on technologies to turn into a component of a comprehensive health care plan.
«For instance, merging AI, machine learning and telehealth together with the IoT-powered remote monitoring tools like wearables, will help healthcare providers track real-time patientsʼ health status, provide accurate diagnosis, treatment decisions, or intervene immediately.»
That is, a truly interconnected care will move beyond isolated video conferences but rather integrated telemedicine will become a part of the digital healthcare systems of flawless triage and referrals between remote and in-person care improving the overall patient journey that matches care to specific needs and optimizes access.
Reinventing the Wheel.. or Embracing the Opportunity?
There are so many other technology-driven trends in digital healthcare. Take the advancement in IoT or precision medicine, robotics, 3D printing, digital platforms with cloud-deployed models, fintech trends marching into the future of healthcare with digital payments and insuretechs literally shaking the whole reimbursement system.
Omitting the shiny things, digital in healthcare can make the continuum of care happen. Clearly, getting these two worlds to blend will not be easy nor flawless. The enthusiasm for a digital change in the domain is confronted with real-life need to strengthen revenue cycle systems that are bound to measure outcomes that affect financial performance today.
The future of digital healthcare is about a paradigm shift to new business models, aka adapting the expectations, altering the approach and welcoming technological entities which is an opportunity to turn it into a value-based care model with an ultimate focus on outcomes that matter to every side. To actively participate in this evolution, companies can develop a healthcare app that aligns with these transformative goals. This involves not only benefits for patients in terms of improved health outcomes and satisfaction, but also providers by helping to diversify revenue sources and improve efficiency. Application development for pharma is a key driver in this shift, enabling pharmaceutical companies to enhance patient engagement, streamline drug distribution, and provide better access to medications through digital platforms.